Blog
12-Lead ECG Placement – Complete Guide
12-Lead ECG Placement and you’d rather not second-guess yourself. Good. Because this isn’t one of those quick “stick on 10 patches and call it done” jobs. The placement matters. Big time. If you get it slightly off, the ECG tracing can mislead you fake signals, missed infarctions, wrong rhythms.
12-lead ECG Placement isn’t just another routine task it’s a small but crucial step in protecting your patient’s physical health. A misplaced lead can easily distort the results, leading to false alarms or, worse, missed warning signs of real cardiac trouble.
This complete guide walks you through everything that matters: how to position each electrode correctly, what common placement errors to avoid, and how to adapt when you’re working with real patients not textbook examples whether they’re overweight, have a hairy chest, or are pediatric cases. By the end, you’ll know exactly how to set up a 12-lead ECG Placement you can trust, with readings that reflect what’s truly happening in the heart.
What is a 12-Lead ECG Placement and why proper placement is vital
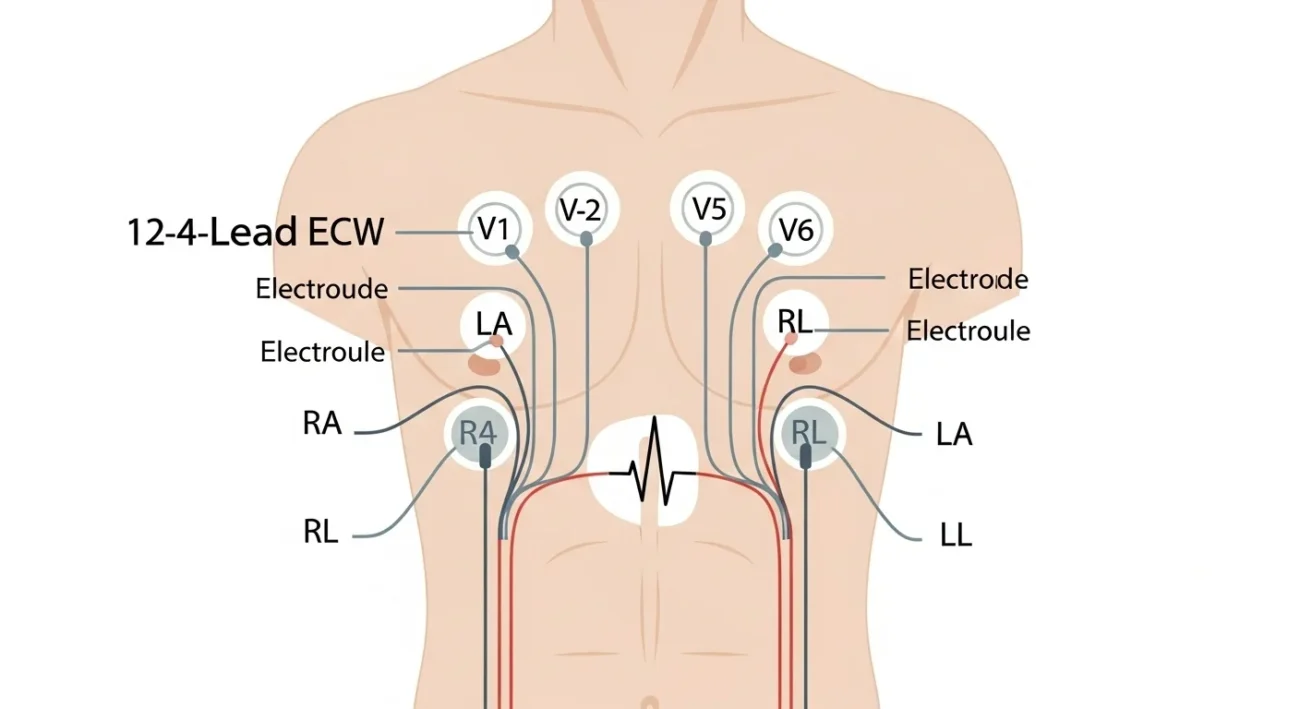
When you hear “12-lead ECG Placement,” it actually means you’re using 10 electrodes (4 limb + 6 chest leads) to create 12 views of the heart’s electrical activity.
Why does placement matter? Because the heart’s electrical signal is tiny. If you slap the chest leads in the wrong intercostal space, or place the limb leads over big muscles instead of proper spots, you’ll change the tracing. That can lead to false positives (for infarction), false negatives, or artefacts that confuse your reading.
So the goal: place leads precisely, get a clean signal, reliable interpretation. Sounds simple until you’re doing it in a hurry, on a sweaty patient, in reduced lighting, with hairy skin. Then the little details matter a lot.
ECG Lead Placement Guide
Master the standard 10-lead configuration for accurate readings
Chest Leads (V1-V6)
V1 Lead
4th ICS, right sternal margin
V2 Lead
4th ICS, left sternal margin
V3 Lead
Between V2 & V4
V4 Lead
5th ICS, mid-clavicular line
V5 Lead
5th ICS, anterior axillary line
V6 Lead
5th ICS, mid-axillary line
Limb Leads (RA, LA, RL, LL)
Right Arm
Right arm (distal)
Left Arm
Left arm (symmetrical)
Right Leg
Right leg (above ankle)
Left Leg
Left leg (symmetrical)
Pre-Placement Checklist
Position patient supine (or semi-recumbent if needed). Arms relaxed at sides.
Clean skin with alcohol wipe or gauze to remove oil, lotion, and dead skin. Rub until area is pink for improved contact.
Trim or shave chest hair where electrodes will be placed. Poor contact = misreading.
Remove jewelry and metal objects from chest and arms area.
Verify electrode tabs and lead wires are correctly connected, not pulling or stretching.
Ensure patient is comfortable and still during recording. Movement creates artifacts.
Skin Preparation Essentials
Clean Surface
Remove oils, sweat, and lotions with alcohol wipes for optimal electrode contact
Hair Management
Trim or shave chest hair at electrode sites to prevent poor signal quality
Accurate Placement
Use anatomical landmarks (ICS, sternal margin) for precise lead positioning
Secure Connection
Ensure electrodes adhere firmly and lead wires aren’t pulling or creating tension
🎯 Quick Tip
ICS = Intercostal Space. Always count from the 2nd rib (at sternal angle) downward. The 4th ICS is crucial for V1 and V2 placement.
Common Mis-placements & How They Mess You Up
You place everything “roughly in the area” and you call it done. That’s when stuff goes sideways.
Example mistakes
- V1/V2 too high (e.g., 3rd ICS instead of 4th) can mimic anterior MI or cause T-wave inversion. Vitali Partners reported up to 50% of cases have this error.
- V4/V5/V6 too low or too lateral leads to altered lateral wall tracing, mis-interpretation.
- Limb leads on torso rather than limbs (or too proximal) changes amplitudes, axis shifts. The AHA guideline warns that torso lead placement cannot be treated interchangeably with standard for serial comparisons.
- Poor skin prep/hair → weak contact → noisy tracing, baseline wander, mis-triggering of machine algorithms.
What this means: you might see ST elevation or depression, Q waves, T-wave changes when in fact none exist. That’s dangerous. Fix the fundamentals.
Adaptations: Dealing with Non-Ideal Patients
Real world: patients aren’t textbook. You’ll face large-breasted women, obese chests, amputees, children, tremors. Here’s how to adapt.
Large-breasted/obese chest
Move V4/V5/V6 leads to the left as necessary you’ll still aim for 5th ICS, mid-clavicular/anterior axillary/mid-axillary lines but you may need to go under the breast tissue or laterally more. Just document it if you deviate. LITFL and others recommend capturing that note.
Children/pediatrics
Smaller patient, but same landmarks apply in principle. For kids in ICU who can’t stay still, limb leads can go on lower abdomen or forearms instead of wrists/ankles.
Tremors/movement/poor preparation
If the patient is shaking (Parkinson’s, cold, jitters), placing limb leads on torso (infraclavicular fo-ssa, costal margin) can reduce artefact but then you must mark the ECG as “modified lead placement” because interpretation will differ.
Amputations or missing limbs
Place the limb electrode as symmetrically as possible: e.g., if left leg is missing, place LL on lower left torso. Document the modification. Then make sure chest placement is perfect because you’ll lean on those leads more.
Why Proper Placement Affects Interpretation
Let’s say you placed V1 and V2 too high. What happens? The septal leads record in a slightly different vector you may get abnormal Q waves or ST changes that suggest septal infarct when there’s none. Mis-diagnosis. Wrong treatment path.
Another example: limb leads on the torso might reduce baseline wander, fine. But they also change the amplitude and duration of QRS and T waves so if you compare this ECG to one done later with standard placement, you’re comparing apples to oranges. The guideline paper says it explicitly: “ECGs recorded with torso limb lead placement cannot be considered equivalent for serial comparison.”
So the takeaway: placement matters because interpretation rests on standardized angles and distances. If you break that standard without noting it, you’re asking for trouble.
What New Info This Guide Gives You
- I show practical skin prep tips (hair, sweat, comfort) which many guides gloss over.
- I list common errors with percentages (e.g., “50% V1/V2 mis-placed”) and focus on how to avoid them.
- I talk about adaptations (chest size, kids, amputations, tremors) and how to document non-standard placement.
- I emphasize the why behind each lead’s location not just “put it here,” but “because this places the vector…”
- I include a placement table you can print out and reference quickly on the job.
FAQs
Q: Can I place limb leads on the torso for faster access?
A: Yes, in some situations (exercise ECG, tremors) you can, but you must mark the ECG as modified. Those results won’t be equivalent to standard limb placement for comparing across time.
Q: Does it matter if V4 is under the breast instead of mid-clavicular line?
A: Yes but the important thing is you stay at the same level (5th intercostal) and note the deviation. Document it. In a woman with large breast tissue, you may place V4 under the breast crest. Competent guidelines accept this.
Q: My patient has lots of chest hair should I shave it?
A: You don’t need to shave a full chest, but trimming the area under each electrode pad helps. Clean the skin, dry it, ensure good contact. Without that, you’ll get noise, loose readings.
Q: I placed V3 after V2 & V4 is that okay?
A: Yes. In fact many guides recommend placing V4 first (since it’s easier to find mid-clavicular line) and then V3 between V2 & V4.
Q: What should I do if the ECG machine says “noisy data”?
A: Check lead wires are not tangled, electrodes are firmly stuck with good contact, patient is still, no muscle movement, dry skin. If limbs tremor or wires pull, relocate leads or use torso limb placement (with documentation).
Conclusion
Okay you’ve got it. The accurate placement of a 12-lead ECG Placement isn’t glam, but it is crucial. The landmarks matter, yes. But so does the prep, the patient context, the documentation. Mistakes happen when we rush or assume “close is good enough.” Close sometimes isn’t.
This guide should give you more confidence. You’ll know where each lead goes, why it matters, what to do when things aren’t ideal, and how to avoid common errors. Print that table. Practice. And next time you hang a 12-lead ECG Placement, you’ll know it’s done right. When you do an ECG, it’s not just wires and stickers it’s the first step in seeing what the heart is trying to tell you. Don’t mess that up.
