Blog
Weakness ICD-10 Code Explained Simply

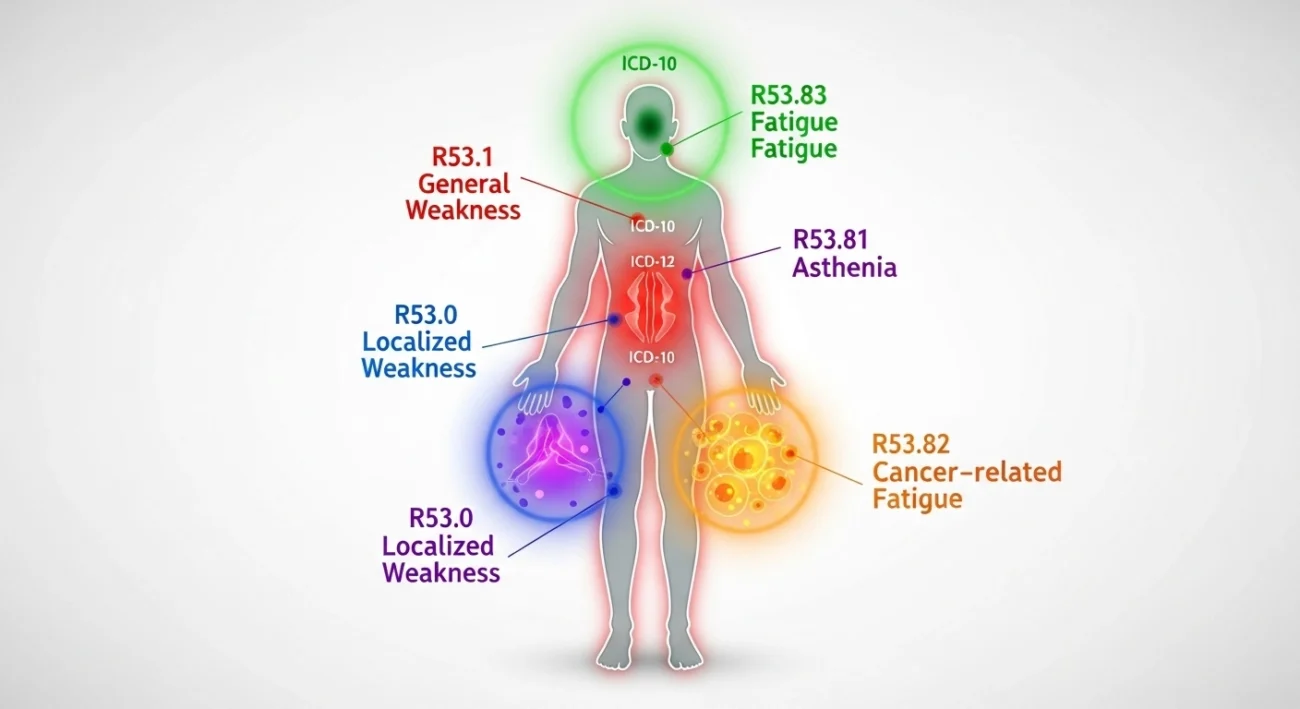
When someone says they feel weak, it can mean anything from mild tiredness’ after a long day, to extreme muscle fatigue that can make it hard to stand, Weakness ICD-10, gurn a heavy object, or even hold a cup. However, in medicine, that one word ‘weakness’ has a distinct meaning that requires documentation. Physicians have to describe it in a format for record keeping, paperwork, and research. One common and simple instance would be the ICD-10 code for weakness (R53.1).
This guide will break down the ICD-10 code for weakness and focus on key points like how it’s used and the reason why it’s accuracy matters so much. Accuracy is essential in this instance. To give you a comprehensive understanding, we will discuss related codes, the way clinicians differentiate genuine muscle weakness and fatigue, common patient misconceptions regarding the word, and so on. This should give you a complete and comprehensive understanding of the working of this word in real life.
Understanding the Weakness ICD-10 Code
The ICD-10 code for general weakness is R53.1. The ICD-10 is a code of classification of every ailment, symptom, and the cause of death created by the World Health Organization (WHO). This classification and coding system is used on an international level.
Code R53.1 is categorized under “Symptoms and signs involving general sensations and perceptions” and is part of Chapter 18 under “Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified.” This simply means weakness/unexplained weakness that a doctor records when no condition is identified. For instance, a patient reports unusual tiredness and weakness and after having some tests a clear diagnosis is not provided, the doctor records R53.1 – Weakness pending further assessment to figure out what the case is.
The Importance of Coding
This process does seem bureaucratic, but these codes do keep modern medicine organized. Each diagnosis, symptom, and procedure performed at a hospital or clinic is identified with one and without appropriate coding, insurance claims could be rejected, public-health monitoring, and research data could become unreliable and even lose precision.
If “weakness” could be documented in a thousand different ways as “muscle tiredness”, “loss of strength”, “low energy”, and so on, patient data could become uncomparable and disorientated across different hospitals or different periods. ICD-10 codes allow the same clinical data to be used across different territories.
General Weakness vs. Fatigue: Why Doctors Care About the Difference
To most people, weakness and fatigue sound identical. But in medicine, they’re not.
- Weakness means a loss of strength. You physically can’t move muscles as powerfully as before.
- Fatigue means feeling tired, even though the muscles still work normally.
For instance, someone with multiple sclerosis or myasthenia gravis might have true weakness because the nerves or muscles aren’t firing properly. On the other hand, someone who’s had too many late nights or is fighting a mild flu might just have fatigue. That difference matters because the ICD-10 code helps define what the doctor is seeing not just what the patient feels.
What Causes Weakness? The Medical View
Weakness can show up for a dozen different reasons. Sometimes it’s temporary, like after an illness, and sometimes it’s an early sign of a more serious condition. Doctors usually group causes into three main categories:
- Neurological causes when nerves or the brain can’t properly signal muscles (for example, stroke, multiple sclerosis, or Guillain-Barré syndrome).
- Muscular causes when the muscle tissue itself is damaged or inflamed (like in muscular dystrophy or polymyositis).
- Systemic or metabolic causes when overall body functions are off, such as thyroid disorders, electrolyte imbalance, anemia, or chronic infections.
In clinical practice, if a doctor can identify the cause, they’ll use a more specific ICD-10 code instead of R53.1. But if the weakness is still unexplained after initial evaluation, R53.1 is the placeholder until more information is available.
How Doctors Decide Which Code to Use
When a patient reports weakness, doctors don’t immediately slap on the code R53.1. They first check:
- Is it generalized or limited to one area?
- Is it due to an underlying condition (like diabetes, stroke, or infection)?
- Is the patient actually weak, or just tired?
Only after ruling out specific causes do they document R53.1 – Weakness. Once tests or follow-ups reveal the cause, the diagnosis and coding are updated.
For example:
- Weakness due to anemia → D64.9 (Anemia, unspecified).
- Weakness from thyroid problems → E03.9 (Hypothyroidism, unspecified).
- Weakness from stroke → I63 (Cerebral infarction).
So, while R53.1 looks simple, it’s often just the first step in a longer diagnostic story.
How Weakness Is Documented and Reported
In healthcare settings, accuracy in documentation isn’t just a formality it affects everything from insurance claims to national health data. For instance, Medicare in the U.S. relies on ICD-10 coding to reimburse doctors correctly.
If a doctor writes “weakness” in a note but forgets to add R53.1, it can delay billing or create confusion in hospital statistics. That’s why even a symptom like weakness gets its own formal code.
Interestingly, a 2023 report from the Centers for Medicare & Medicaid Services (CMS) highlighted that “unspecified” symptom codes like R53.1 remain among the most frequently used in outpatient visits (CMS, 2023). It’s a reminder that even common, vague symptoms carry real weight in clinical data.
When Weakness Isn’t Just Weakness
Sometimes weakness is the body’s early warning system. Chronic weakness might point to long-term issues like:
- Nutrient deficiencies (low iron or B12).
- Autoimmune conditions that affect muscles.
- Endocrine disorders like diabetes or adrenal fatigue.
- Nerve compression or damage.
Research published in The Journal of the American Geriatrics Society (2021) found that persistent weakness in older adults often predicts mobility decline and higher hospitalization risk. It’s not just an inconvenience it’s a measurable sign of declining health.
That’s why primary care physicians take even vague “feeling weak” complaints seriously, especially in older patients or those with chronic diseases
Can General Weakness Be Prevented?
Sometimes, yes. The key is treating the underlying cause or improving overall energy balance.
- Stay hydrated: Even mild dehydration reduces muscle performance (European Journal of Applied Physiology, 2020).
- Balanced diet: Iron, vitamin D, and protein levels play a major role in maintaining strength.
- Regular movement: Light resistance training and walking improve muscle endurance and help prevent disuse weakness.
- Sleep: Poor sleep disrupts muscle recovery and can mimic fatigue or weakness (Sleep Medicine Reviews, 2022).
While R53.1 describes weakness as a symptom, prevention and management depend on addressing what’s really driving it.
The Takeaway
R53.1 – Weakness might seem like a small line on a medical chart, but it captures one of the most common reasons people visit doctors. It’s a bridge between how a patient feels (“I feel weak”) and how medicine classifies that experience for diagnosis and care.
By understanding what the ICD-10 code means, you not only read your medical paperwork with more confidence but also see how modern healthcare translates everyday language into structured, global data.
If there’s one thing to remember, it’s this: weakness isn’t a diagnosis it’s a clue. That code (R53.1) is where the story begins, not where it ends.
References
- World Health Organization. ICD-10: International Statistical Classification of Diseases and Related Health Problems (10th Revision). WHO, 2019.
- Centers for Medicare & Medicaid Services (CMS), Top 50 ICD-10 Codes in Outpatient Visits, 2023.
- Journal of the American Geriatrics Society, 2021 – “Muscle Weakness as a Predictor of Functional Decline in Older Adults.”
- European Journal of Applied Physiology, 2020 – “Impact of Hydration on Muscle Performance.”
- Sleep Medicine Reviews, 2022 – “Sleep Quality and Physical Function in Adults.”
