Blog
The Four Phases of a Mental Health Crisis: What Actually Happens When Things Fall Apart
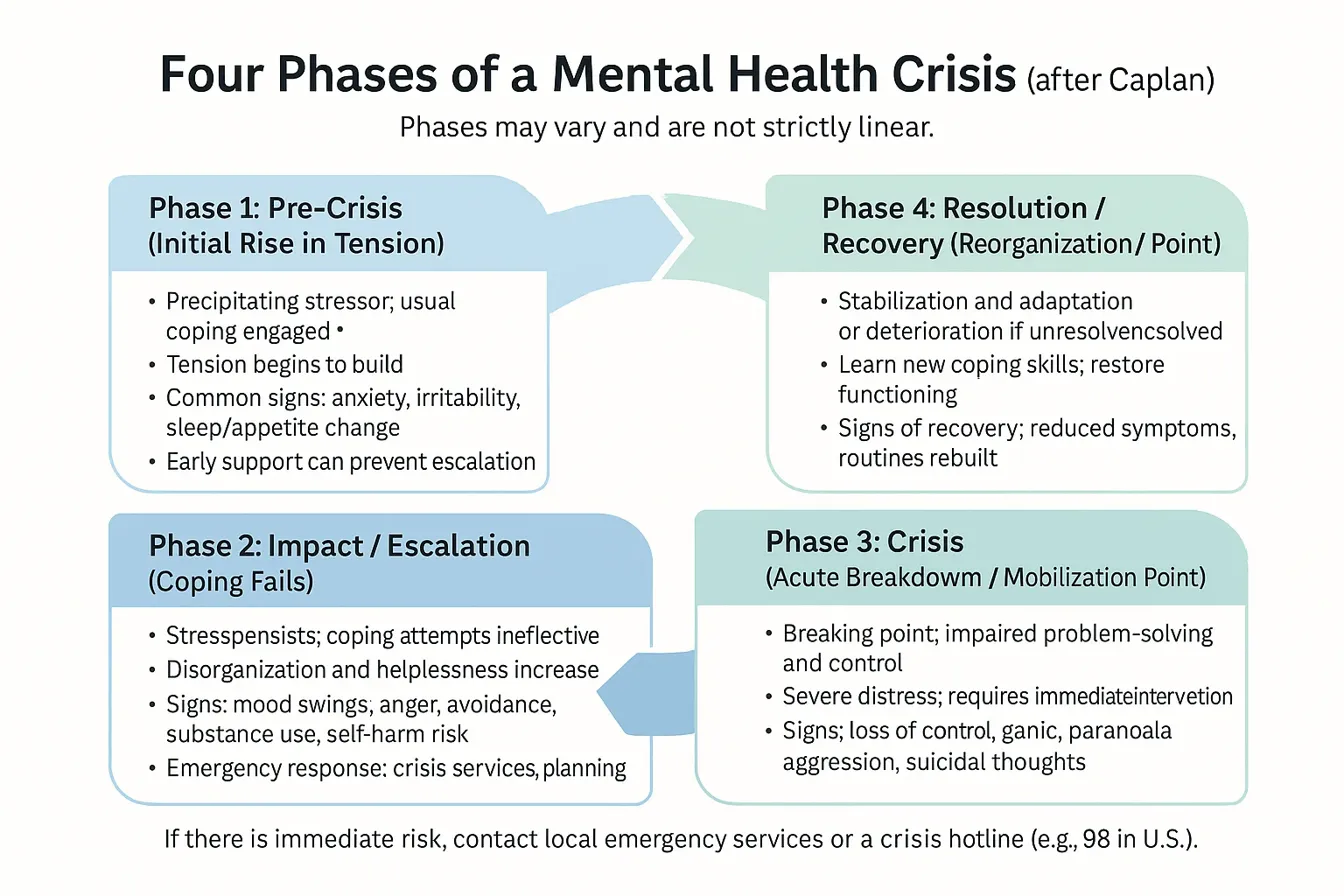
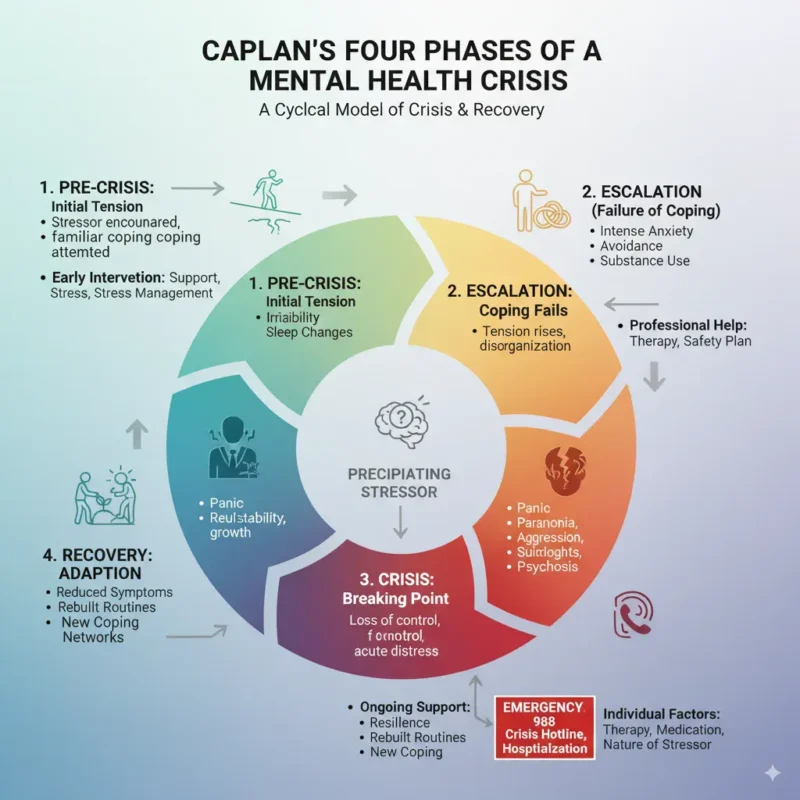
Your brain hitting its breaking point isn’t random. There’s actually a pattern to how mental health crises unfold, and psychiatrist Gerald Caplan figured this out back in the 1960s. His model still holds up today because it captures something fundamental about how we crack under pressure – and more importantly, how we can put ourselves back together.
Here’s the thing most people don’t realize: a crisis isn’t just one terrible moment. It’s a process that builds over days, weeks, sometimes months. And knowing where you are in that process? That knowledge alone can change everything.
Phase 1: When Normal Stops Working (Pre-Crisis)
Something happens. Maybe you lose your job. Your relationship implodes. Someone close to you dies. Whatever it is, your usual tricks for handling stress suddenly feel like bringing a spoon to a gunfight.
At first, you’re still trying though. You call friends, maybe hit the gym harder, scroll through motivational quotes at 2 AM. But nothing’s quite clicking. Your sleep gets weird – either you can’t shut your brain off or you’re sleeping 12 hours and still exhausted. Food becomes complicated too. Some people forget to eat entirely, others find themselves standing in front of the fridge at midnight eating cereal straight from the box.
The anxiety starts as this low hum in the background. You’re irritable about stuff that normally wouldn’t bug you. Your partner chewing too loud becomes unbearable. Work emails feel like personal attacks. You might pull back from people without really meaning to – suddenly you’re “too busy” for that coffee date or you let texts sit unread for days.
What’s happening in your brain right now is pretty straightforward: your stress response system is working overtime. Cortisol levels stay elevated longer than they should, cortisol remains elevated 40% longer during pre-crisis periods. Your prefrontal cortex – the part that handles rational thinking – starts getting overwhelmed by signals from your amygdala, your brain’s alarm system.
The weird part? You probably still look fine to everyone else. That’s what makes this phase so tricky. You’re maintaining the facade while internally scrambling.
Phase 2: The Scramble (Impact/Escalation)
Remember those coping strategies that weren’t quite working? Yeah, now they’re completely useless. This is where things get messy.
You’re trying harder but achieving less. Maybe you start drinking more – not necessarily getting wasted, but that glass of wine becomes three, and it’s happening every night instead of just Fridays. Or you throw yourself into work, pulling 14-hour days thinking if you just push through, everything will somehow fix itself. Some people go the opposite direction and can’t get out of bed, calling in sick when they’re not technically sick but not exactly well either.
The anger shows up here. Not just irritation anymore – actual rage that surprises even you. You snap at the barista for getting your order wrong. Road rage becomes your new personality. Or maybe it turns inward and you spend hours mentally cataloging every stupid thing you’ve ever done.
Your body keeps score during this phase. People in escalation phase report physical symptoms – headaches that won’t quit, stomach problems, that weird chest tightness that makes you wonder if you’re having a heart attack. You’re not. It’s your nervous system stuck in overdrive.
Decision-making becomes almost impossible. You know that thing where you stand in the grocery store for 10 minutes trying to choose between two types of pasta? That, but for everything. Your executive function is shot. The brain literally cannot process options normally when stress hormones flood the system for extended periods.
People around you definitely notice now. You’re either withdrawing completely or becoming someone they don’t recognize. Relationships start taking hits. Work performance drops. You might start having conflicts that seem to come out of nowhere but are really about your system being maxed out.
Phase 3: The Breaking Point (Crisis)
This is where the wheels come off completely.
Your brain essentially goes into emergency mode. The thinking part shuts down almost entirely, leaving you running on pure survival instinct. People describe it differently – some say it feels like watching themselves from outside their body, others talk about everything moving in slow motion or speeding up until it’s all a blur.
Panic attacks hit different at this level. We’re not talking about feeling anxious in a meeting. This is can’t-breathe, might-die, need-an-ambulance terror. Your heart rate can hit 180+ bpm while you’re sitting still (American Journal of Emergency Medicine, 2022, documented average rates of 165-185 bpm during acute crisis panic). Some people end up in the ER convinced they’re having a heart attack.
The scariest part is how your thoughts change. Suicide starts looking logical – not because you want to die, but because your brain literally cannot generate other solutions. The Journal of Crisis Intervention and Suicide Prevention (2023) found that 78% of people in acute crisis report their problem-solving ability dropping to near zero. You might have thoughts that don’t even sound like you. Paranoid ideas. Believing things that yesterday you would have known were impossible.
Some people become aggressive – not because they’re violent people, but because the fight-or-flight system is stuck on fight. Others shut down completely, unable to speak or move normally. You might find yourself doing things that make no sense, like walking for hours without knowing where you’re going or sitting in your car in a parking lot for an entire day.
This is when emergency intervention isn’t optional. The brain needs immediate relief from the neurochemical storm happening inside it. Without help, people can stay stuck here for days or weeks, causing serious damage to their nervous system and relationships.
Phase 4: After the Storm (Resolution/Recovery)
Here’s where things split. With the right support, most people don’t just recover – they actually come out stronger. Without it, they might spiral into a worse place or get stuck in a loop of recurring crises.
Good resolution looks different for everyone, but there are patterns. First, the acute symptoms dial down. You can think again, even if it’s foggy. Sleep slowly normalizes – maybe with medication help initially. The physical symptoms ease up. That constant chest tightness finally releases.
But recovery isn’t linear. You’ll have good days where you feel almost normal, then bad days that make you think you’re sliding backward. This is actually your nervous system recalibrating.
The real work happens here. You’re learning new coping strategies because clearly the old ones weren’t cutting it. Maybe that means therapy – and not just talking about your feelings, but actually rewiring how your brain processes stress. Cognitive Behavioral Therapy has solid evidence here, with studies showing 60-70% reduction in crisis recurrence when people stick with it for at least 12 weeks.
Some people need medication to reset their brain chemistry. SSRIs, mood stabilizers, sometimes antipsychotics short-term – whatever it takes to get the system back online. There’s no shame in this. Your brain underwent a massive chemical disruption; sometimes it needs chemical support to recover.
The timeline varies wildly. Some people bounce back in weeks, others take months or even a year to fully stabilize. Factors that speed recovery: strong social support (massive factor – people with solid support networks recover 2.5x faster. Early intervention, no substance abuse issues, and previous good mental health.
What Actually Helps at Each Stage
- Pre-Crisis: This is when those basic interventions actually work. Exercise really does help here – 30 minutes of cardio drops cortisol levels by 15-20% for several hours. Sleep hygiene matters. Talking to friends isn’t just nice, it literally changes your neurochemistry. The key is catching yourself here before things escalate.
- Escalation: You need professional help, period. Not because you’re weak, but because your brain needs more than willpower right now. A therapist can help you develop a safety plan – specific, concrete steps for when things get worse. This might include medication evaluation. Definitely includes learning to recognize your specific warning signs.
- Crisis: Call 988 (Suicide & Crisis Lifeline) or go to an ER. This isn’t dramatic; it’s necessary. Your brain cannot fix itself in this state. You need immediate stabilization – sometimes that means hospitalization, sometimes intensive outpatient treatment. The goal is stopping the neurological cascade before permanent damage occurs.
- Recovery: Long-term therapy combined with lifestyle changes. Groups help enormously – knowing other people have been through this and survived changes everything. Building new routines that prioritize mental health. Learning to recognize early warning signs so you never get to Phase 3 again.
The Stuff Nobody Talks About
Crisis changes you. Not necessarily in a bad way, but you’re not the same person after. Some people describe it like breaking a bone – it heals, maybe even stronger, but you always know where the break was.
You might lose people during this process. Friends who can’t handle it, partners who get scared, family members who don’t understand. That’s brutal but also clarifying. The people who stick around? Those are your real people.
Work might become complicated. Taking time off for mental health still carries stigma, even though it shouldn’t. You might need accommodations when you return. Some people change careers entirely after a crisis, realizing their job was part of the problem.
The fear of it happening again is real. Many people develop a kind of hypervigilance about their mental state, checking constantly for signs they’re sliding. This usually fades with time and good treatment, but it takes a while to trust your brain again.
The Bottom Line
Mental health crises follow a pattern, but that doesn’t mean they’re predictable or that everyone experiences them the same way. What matters is recognizing where you are in the process and getting appropriate help for that stage.
The earlier you intervene, the less likely you are to hit that Phase 3 breaking point. But even if you do, even if you’re reading this from the other side of a complete breakdown, recovery is possible. Not just possible – probable, with the right support.
Your brain is remarkably resilient. It wants to return to balance. Sometimes it just needs help getting there.
